2023-2025
Morphological analysis of intracranial pressure and arterial blood pressure pulse waveforms using deep learning
Project leader: Agnieszka Kazimierska, PhD
PRELUDIUM 21 programme, National Science Centre, Poland, grant UMO-2022/45/N/ST7/01980
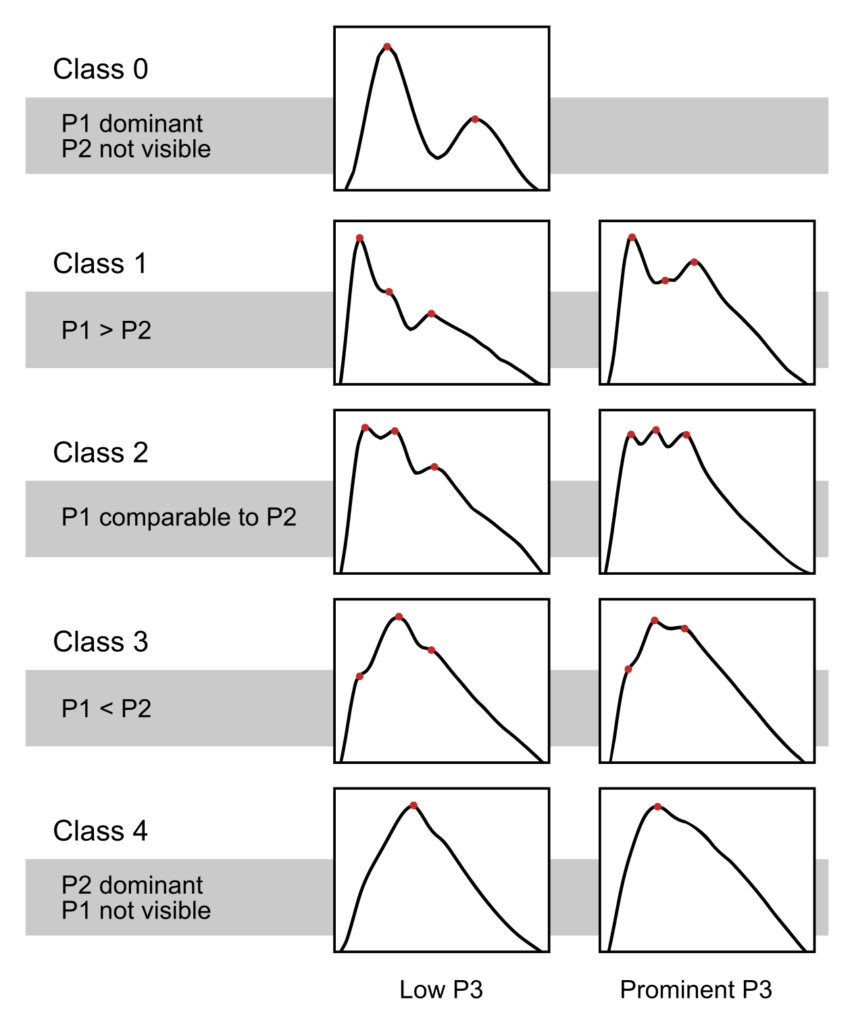
Traumatic brain injury (TBI) is one of the leading causes of death and disability worldwide, affecting both young people (mostly as a result of traffic accidents and violence) and the elderly (mostly as a result of falls). In addition to expensive hospitalisation and treatment, TBI is associated with significant socioeconomic costs as TBI patients often have to undergo long-term physical therapy, require assistance with everyday activities and may not be able to return to work. Due to its complex nature, which includes both primary injury to the brain and a large number of secondary complications, management of TBI patients is very difficult and the subject of ongoing study. Numerous scientists and clinicians over the years have tried to improve our understanding of the factors influencing the patient’s condition and propose new diagnostic and therapeutic tools that would prevent it from worsening, reduce mortality and limit the negative effects of brain injury on the patient’s life after hospitalisation. Intracranial pressure (ICP) is one the most important signals monitored in TBI patients in modern neurointensive care units. ICP elevation is considered a life-threatening complication that may result in secondary damage to the brain and increase the risk of death. However, current clinical protocols are mostly based on observation of mean ICP value and therapy is usually introduced after ICP increases have already happened, which means that it may not be sufficient to prevent the damage from taking place. It has been proposed a long time ago that existing management strategies may be improved by assessing the cerebrospinal system’s ability to compensate changes in intracranial volume without potentially dangerous increases in pressure, which would allow for identification of TBI patients at risk of intracranial hypertension before the rise in ICP manifests. The ICP pulse waveform, which is the change in the ICP signal that occurs over a single cardiac cycle, has been shown to change shape with decreasing volume buffering capacity. Under normal conditions, it resembles a saw-tooth with three defined local maxima. As the compensatory reserve decreases, it becomes rounded and only one of the maxima remains visible. Recently, we showed that different shapes of the ICP pulse waveform can be automatically classified on scale from normal to pathological using artificial intelligence methods and that the occurrence of pathologically changed pulses is higher in patients who died after TBI, which supports the potential of using this method to improve the management of TBI patients.
However, the ICP pulse waveform is also influenced by other factors besides the compensatory reserve and its source is believed to lie in arterial pulsations which travel through blood vessels to the craniospinal compartment. As TBI may involve severe disturbances in the circulatory system, we hypothesise that ICP pulse waveform analysis may also reflect the vascular factors that define the shape of the arterial blood pressure (ABP) pulse and the two signals should be assessed in parallel to obtain a precise description of the patient’s condition.
In this project we aim to extend our previous studies by analysis of the ABP pulse waveform and classify characteristic shapes of both ICP and ABP pulses observed in TBI patients using artificial intelligence methods. The classification models we will develop will offer new tools to study the changes in physiological signals monitored in TBI patients after injury. We plan to investigate the ICP pulse shape in relation to the ABP signal in order to evaluate the possible effect of vascular factors on the intracranial pressure–volume relationship. Moreover, we intend to examine the link between the occurrence of different patterns of ICP and ABP pulses and the clinical status and outcome of TBI patients. This analysis will improve our understanding of the processes that occur in the cerebrospinal space after TBI and allow us to characterise the patient’s condition more accurately. This in turn will offer new insight into the significance of changes observed in the ICP and ABP pulse waveforms and their importance for prediction of the patient’s outcome.
Publications:
- Kasprowicz, M., Mataczyński, C., Uryga, A., Pelah, A.I., Schmidt, E., Czosnyka, M., Kazimierska, A., & CENTER-TBI high-resolution sub-study participants and investigators (2025) Impact of Age and Mean Intracranial Pressure on the Morphology of Intracranial Pressure Waveform and Its Association with Mortality in Traumatic Brain Injury. Critical Care, 29 art. 78. https://doi.org/10.1186/s13054-025-05295-w
- Mataczyński, C., Kazimierska, A., Beqiri, E., Czosnyka, M., Smielewski, P., Kasprowicz, M., & CENTER-TBI high-resolution sub-study participants and investigators (2025) Interpretable Model Committee for Monitoring and Early Prediction of Intracranial Pressure Crises. Expert Systems With Applications, 265 art. 126001. https://doi.org/10.1016/j.eswa.2024.126001
- Kazimierska, A., Manet, R., Vallet, A., Schmidt, E., Czosnyka, Z., Czosnyka M., & Kasprowicz, M. (2023) Analysis of Intracranial Pressure Pulse Waveform in Studies on Cerebrospinal Compliance: a Narrative Review. Physiological Measurement, 44 art. 10TR01. https://doi.org/10.1088/1361-6579/ad0020
Conference presentations:
- Kazimierska, A., Mataczyński, C., Czosnyka, M., Kasprowicz, M., & CENTER-TBI high-resolution sub-study participants and investigators. Changes in intracranial pressure pulse waveform morphology associated with intracranial pressure and arterial blood pressure. 2024 Meeting of the International NeuroTrauma Society (INTS 2024), 2–5.09.2024, Cambridge, UK.